This is not my typical blog post, but a paper I had to write for my GCU nursing class. Since much of my creative juices are currently being directed toward nursing school, I figured I might as well publish some of my work here on my blog!
Moving Along the Illness-Wellness Continuum over a Lifetime
Danielle Tantone
Department of Nursing, Grand Canyon University
NRS-434VN: Health Assessment
Geraldine Bazzell, RN, MSN
1/31/21
Just over a year ago, I was enjoying a peaceful September afternoon at the park with my youngest daughter in the midst of a crazy stressful life: three kids, nursing school, working nights at the hospital as a nursing assistant.
The blazing summer heat had broken, and it was finally cool enough to enjoy the outdoors in Arizona. My cell phone rang, and my doctor gave me the life-changing news that I had breast cancer. But I was neither shocked nor alarmed. I was high-risk and had gone in for a biopsy two days earlier after my mammogram showed some microcalcifications.
I had done my research, so when she told me that the biopsy had revealed high grade, Stage 0 ductal carcinoma in situ, the earliest form of breast cancer, my mind went right toward making a plan and focusing on all the silver linings, of which there were many.
I had just turned 45 and I was at a healthy weight, eating a healthy diet and exercising regularly. I decided almost immediately that the best treatment option for me was a bilateral mastectomy with reconstruction. Yes, I could have chosen “just” a lumpectomy, but by choosing the double mastectomy I avoided chemotherapy, radiation and even hormone therapy, all of which, to me, were far more invasive than simply removing the breasts which had served me well but were no longer strictly necessary.
I believe that the healthy mental attitude I chose to adopt during this health ordeal was just as important as my physical health, and despite my serious disease diagnosis, I stayed in a state of overall wellness throughout the entire ordeal.
Wellness has many components: physical, mental and emotional. Though it can be pictured as a continuum, along which we all move back and forth throughout our lifetimes, it is actually a multi-dimensional concept that is hard to completely understand on a one-dimensional model. One can be sick in terms of disease, but rate high in terms of overall wellness, or one can be free of disease but not enjoying a state of overall wellness at all (Wellness, 2018).
The goal is to be not just free of disease, but in a state of optimal wellness as much as possible over the course of a lifetime. As nurses, it is important to be aware of our patients’ – and our own overall state of wellness and not simply look at whether or not we are experiencing symptoms of disease.
The origins of the Illness-Wellness Continuum
The health-illness continuum, originally conceived and published by John Travis, MD, MPH in the 1970s, provided a nice picture to show how optimal wellness was achieved by moving past simple absence of disease to higher levels of wellness. The idea was a combination of the Lewis Robbins’ health risk continuum created by Lewis Robbins and Abraham Maslow’s concept of self-actualization.
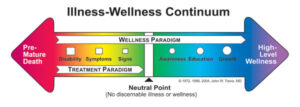
However, the model makes it hard to understand the fact that it is possible to be physically ill but oriented toward wellness, or physically healthy but suffering from an illness mentality, and the continuum is rarely a perfect line. Even if someone is sick, in a disease state, they can still be doing very well in terms of overall wellness (Wellness, 2018).
More About the Illness-Wellness Continuum and Travis’ Work
Moving from the center to the left shows a progressively worsening state of health, while moving to the right of center indicates increasing levels of health and wellbeing. While medical treatment such as drugs, herbs, surgery, psychotherapy, etc. alleviates symptoms and brings a patient to the neutral point, the wellness paradigm can be utilized at any point on the continuum, and directs a patient beyond neutral. This idea of true wellness does not replace treatment, but works in harmony with it (Wellness, 2018).
A state of emotional stress can lead to physical and mental disease, even cancer, and true wellness is not a static state. In fact, it’s not as important exactly where a patient falls on the spectrum so much as in which direction he is headed. Even dying can be done from a place of wellness (Wellness, 2018).
The Importance of Understanding the Continuum in Patient Care
The health-illness continuum also interacts with the continuum of patient care. In a healthcare system that is often criticized for focusing on acute conditions rather than wellness and prevention, thinking of wellness in terms of a spectrum has advantages for everyone involved. A truly patient-oriented system of care “spans an entire lifetime, is composed of both services and integrating mechanisms, and guides and tracks patients over time through a comprehensive array of health, mental health, and social services across all levels of intensity of care” (American Sentinel University, 2020).
Such a system would provide high-quality and cost-effective care for patients using community-based services such as home health nurses, telemedicine, disease management programs, informatics, and case management. Nurses are essential within this continuum of care. They support treatment, help educate and guide their patients toward better health outcomes (American Sentinel, 2020).
Nurses must consider not only the continuum of care, but also pay attention to where each patient is within his own health-illness spectrum, always remembering to look at the patient holistically. A nurse’s role goes far beyond simply treating disease. She can have a tremendous value in promoting overall wellness on every level.
Nurses’ Personal Place Along the Health-Illness Continuum
On another note, nurses must pay close attention to where they, themselves are along the continuum as well, since they can’t very well take care of others if they aren’t taking care of themselves first. Studies have shown that nurses experience more musculoskeletal disorders, depression, tuberculosis, infections and occupational allergies than the general public. Nurses’ shift work was shown to lead to sleep deficiency, lack of exercise, cardiological and metabolic problems, and even cancer (Letvak, 2014).
And while the nurses’ health is important, it is not just about them. Studies also show that nurses who work with physical and mental illness experience more medication errors and patient falls, and offer an overall lower quality of patient care provided (Letvak, 2014).
According to the ANA, “A healthy nurse lives life to the fullest capacity, across the wellness/illness continuum, as they become stronger role models, advocates, and educators, personally, for their families, their communities and work environments, and ultimately for their patients” (Letvak, 2014).
The ANA offers many levels of support for nurses on their own journey along the health-illness continuum.
Health is in a Constant State of Change
A person’s health is always in a state of continual change on every level, moving from health to illness and back again. His condition is rarely constant. The health-illness continuum (see figure 1-1) illustrates this process of change. Each individual experiences various states of health and illness throughout his life. But it is actually the individual’s response to the change, rather than the change itself, that affects his health most profoundly (Brookside, 2015).
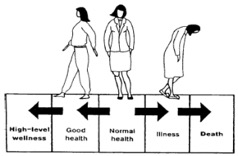 Figure 1.1 (Brookside, 2015)
Figure 1.1 (Brookside, 2015)
Adaptation to a chronic disease can be considered a state of wellness. If one person is in great physical condition, but suffering from depression or substance abuse and unable to go to work, while another is living with a chronic disease like diabetes but functioning fully within his life, which one is at a higher level on the health-illness continuum (Brookside, 2015)?
Where I See Myself on the Continuum
I have always thought of myself as an overall healthy person. I know my body well and I take care of it. However, I have not ruled out the possibility that the physical and emotional stress I was under in 2019 actually led to my breast cancer. I was dealing with a lot and I was working the night shift, which has been proven to throw off the body’s circadian rhythm. Some studies even show a link between shift work and cancer (Yuan, 2018).
So, in that moment, I was heading toward illness. However, the fact that I was being regularly screened and took prompt action to treat the cancer, and the fact that I chose to see all the blessings in my diagnosis turned me around toward the wellness end. Facing illness with eyes wide open, trusting God and having a strong support system are huge in terms of wellness.
Conclusion
As an aspiring nurse, I find it encouraging that we are learning about the health-illness continuum. I feel very strongly that good healthcare is so much more than simply eliminating disease. As nurses, we can have an impact of the overall wellness of our patients and the entire community. The patient care experience, like the human experience itself, is about so much more than just staving off disease. Nurses can have an impact on a person’s entire life through their compassionate caring, empathy, education and love. A good nurse can encourage, inspire and comfort her patients, promoting dignity in the most embarrassing of situations and helping a patient turn back in the direction of wellness no matter how sick they are.
It is important that nurses do not forget to treat themselves as their most important patient, taking care to get enough sleep, exercise, healthy food and mental, emotional and spiritual stimulation. It is a stressful and important job we do. We hold our patients’ lives in our hands. We must never take our own health for granted or think that it is unimportant.
I am grateful that I got cancer. I am glad I got to experience what it is like to be a patient. I am grateful that they caught it early and that through my journey, I have been able to encourage so many others – to get regular screenings, to not be afraid of bad news, but to welcome it because getting the news lets them do something to fix it, and to face their challenges with grace and faith.
References
American Sentinel University. (2020). What is the Healthcare Continuum of Care and What Are the Different Nursing Roles Within it? The Sentinel Watch. Retrieved from https://www.americansentinel.edu/blog/2020/02/15/nursings-role-in-the-continuum-of-care/
Brookside. (2015). The Health-Illness Continuum. Nursing Fundamentals 1. Distance Learning for Medical and Nursing Professionals. Retrieved from https://brooksidepress.org/nursing_fundamentals_1/?page_id=115
Letvak, S. (2014). Overview and Summary: Healthy Nurses: Perspectives on Caring for Ourselves. OJIN: The Online Journal of Issues in Nursing Vol. 19, No. 3, Overview and Summary. Retrieved from https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-19-2014/No3-Sept-2014/OS-Healthy-Nurses.html
Wellness Associates. (2018). Key Concept #1: The Illness-Wellness Continuum. Retrieved from http://www.thewellspring.com/wellspring/introduction-to-wellness/357/key-concept-1-the-illnesswellness-continuum.cfm.html
Yuan, X., Zhu, C., Wang, M., Mo, F., Du, W., Ma, X. (2018). Night Shift Work Increases the Risks of Multiple Primary Cancers in Women: A Systematic Review and Meta-analysis of 61 Articles. Cancer Epidemiology, Biomarkers & Prevention. Retrieved from https://cebp.aacrjournals.org/content/27/1/25
Danielle,
Thank you for sharing about your diagnosis and a bit about your journey with breast cancer; this is a perfect example of how emotional health impacts our placement on the continuum. Good discussion of each section of the assignment. This is one of the best submissions I have had for this assignment. See comments throughout for learning opportunities.
Geri

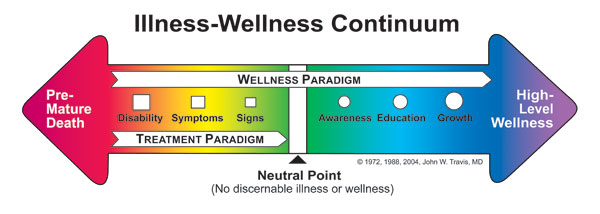
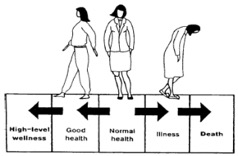 Figure 1.1 (Brookside, 2015)
Figure 1.1 (Brookside, 2015)